Melbourne urologist
prostate conditions
Prostate problems
What is the prostate?
As a man, your prostate is a small, soft gland located in your pelvis. It is about the size of a walnut or a ping pong ball, and it is located between your bladder, the base of the penis and in front of the rectum. The prostate surrounds a segment of the tube that delivers urine from the bladder to the outside world (the urethra).
In men, the prostate gland is important for reproduction. Its growth is regulated by hormones such as testosterone. It produces about a third of all the fluid in your semen while the other components are produced in your testes. The prostate gland contains vital enzymes that help your semen survive during reproduction.
What is non-cancerous prostate disease?
Non-cancerous prostate disease
Prostate conditions: enlarged prostate
Enlarged prostate
Enlarged prostate is a condition often seen in men over 50. You will hear the scientific medical term ‘benign prostatic hyperplasia’ or the abbreviation BPH being used to describe it.
Most men will experience some enlargement of their prostate gland, and in some cases, it may even be as much as triple in size or larger.

‘It is important to remember that prostate enlargement is not cancer. Almost half of the men over 60 and 80% of men over 70 have it. Prostate cancer on the other hand usually does not cause the typical obstructive symptoms.’
Reduced urine flow is often the main symptom and the reason why you would come to see me as your urologist. Your prostate surrounds the tube that transports urine, and that is why the first symptoms of enlarged prostate will be linked to the passing of urine.
In short, symptoms of enlarged prostate include:
- A weak urinary stream (the flow deteriorates or stops and starts)
- Difficulty starting urination
- Dribbling at the end of your stream
- Waking up at night to pass urine
- Sensation of incomplete emptying of your bladder
- Urgency – unable to hold on or needing to go when you need to go
- Frequency – Needing to pass urine often
- Blood in the urine
- Urine tract infections
- Inability to pass urine
Do I need to see a doctor for an enlarged prostate?
If you experience any of the symptoms, it is worth getting evaluated by your GP or a urologist. That is important because the obstruction to your urine flow can increase the risk of urine infections, bladder stones and bladder weakness or kidney function. The reason is that an enlarged prostate causes pressure on your bladder and kidneys.
If you are suddenly unable to pass urine, then it is urgent to see your urologist or seek emergency medical care as this can lead to serious complications including kidney damage.
So what will I do when you come to see me as your urologist?
- I evaluate your symptoms. We take the time to discuss them in detail so I get a full understanding of your condition. For me, it is not just about the diagnosis and the test results. It is about how prostate problems may affect your overall health and your daily life. We will make sure there are no other concerning causes for your symptoms such as cancer, try to identify what symptoms bother you the most and take action to address them.
- We plan a clinical evaluation to assess the size and the consistency of your prostate gland. This happens through a digital rectal exam.
- Further evaluation happens with an ultrasound scan. It assesses your prostate, your bladder, how much is left in your bladder and we may also measure the flow of your urine.
- A blood test can be used to assess your kidney function.
- Other tests may be planned to rule out infections, prostate cancer (PSA Test), narrowing of the urethra, scarring, or other conditions that affect your urine flow.
Do I need treatment for an enlarged prostate?
We map and assess your symptoms and this information will define the course of treatment. Your lifestyle and the exact size of your prostate are other factors. The main goal of treatment is to relieve the obstruction caused by your prostate and to reduce the compression of your urethra.
When we discuss your condition, I use my experience and the available research to help you make a well-informed choice.
There are medical treatments to reduce the size of the prostate and improve the symptoms.
The surgical treatment options for an enlarged prostate include:
- Urolift (opening the prostate using staples).
- Procedures to evaporate the prostate using laser (Green light) or water vapor (Rezum).
- Removing the obstructing segment of the prostate (transition zone) by using electrocautery (TURP) or laser (Holep).

Melbourne urologist Prostatitis
Prostatitis: What is it?
- Burning or stinging when you pass urine
- Cloudy urine or blood in your urine
- Difficulty passing urine
- Pain in the pelvic area
- High fevers or flu-like symptoms including fevers, chills, body aches, nausea or vomiting
Do I need treatment for prostatitis?
My role as your urologist is to help you understand the type of prostatitis that you may have. We look at the symptoms, and we plan the routine tests to get clear about your condition. Then we take the type to discuss the treatment options.- Home remedies such as hot baths, hot water bottles, and relaxation exercises.
- Dietary changes such as avoiding spicy food, coffee, tea and alcohol which can all irritate your bladder and increase the urinary symptoms. Drinking more water can be helpful.
- Lifestyle changes such as avoiding bicycle riding which can worsen symptoms
- Visiting a physiotherapist can be useful and they can teach Kegels exercise and biofeedback.
- Acupuncture has also shown to be effective.
Melbourne urologist prostate cancer
Prostate cancer
Prostate cancer is an uncontrollable growth of the cells that make up the prostate. The risk of prostate cancer increases with age and often affects men aged 60 and above, or men who have a close relative with prostate or breast cancers.
Research shows that prostate cancer is the most common cancer in Australian men with an estimated 1 in 5 men being diagnosed with prostate cancer. However, not all prostate cancers are the same. While some cancers are fast-growing and spread fast, other types of prostate cancer have slow growth.
Prostate cancer also has a 95% 5-year survival rate and that is why early identification of prostate cancer offers the best outcomes. As your urologist, I can then determine the need for treatment in an early stage.
The PSA test is commonly used to detect prostate cancer in men, and an elevated level may warrant further evaluation. Apart from prostate cancer, there are many other reasons why your PSA level may be elevated.
What is a raised PSA?
PSA or ‘Prostate Specific Antigen’ is an enzyme produced by the prostate gland. PSA can also be detected on a blood test.
Although raised PSA is often associated with prostate cancer, PSA levels can be raised due to a number of reasons including:
- Urine or prostate infection
- Enlarged prostate
- Masturbation
- Cycling
- Vigorous exercise
- Prostate examination (Digital rectal examination)
- Recent urologic procedure
Should you get a PSA test?
PSA screening is controversial but in clinical studies, it is shown to reduce the number of deaths from prostate cancer by up to 21% at 13 years of follow-up. That means that, for every 27 men that are diagnosed with prostate cancer after a PSA test, one life is saved. It is important to note that screening also comes with some potentially harmful effects. You may have heard the expression that ‘Most men die with prostate cancer rather than from it’. It refers to research and to the fact that a large proportion of the prostate cancers detected do not need treatment. They still need careful observation.- If you are 45 – 69 years you could opt to get PSA tests every 2 years as long as you are aware of the benefits and harms associated with the testing.
- If you have a strong family history of prostate cancer or breast cancer with multiple immediate family members who were diagnosed at a young age, getting your first PSA test at the age of 40 is recommended. Otherwise, there is no benefit in getting PSA tests prior to the age of 40.
- The frequency of PSA testing may be determined by the doctor, for instance, if you are aged 45 and the initial PSA is normal.
- Abstain from masturbation or sex 48 hours prior.
- Avoid vigorous exercise including cycling for the 48 hours prior.
What to do if you have an elevated PSA test?
It is good to be aware of what is considered normal and abnormal when you discuss your PSA test results with your urologist. I am here to help you understand what the test results are telling us, to make sure that you are clear. That includes knowing when treatment is advised, and when to avoid excessive worrying.How is prostate cancer diagnosed?

‘With usually no obvious symptoms to guide us, we rely on a PSA test and also a prostate examination through the rectum which allows us to feel for any abnormalities on the outside of the prostate’
If I have a concern after a digital rectal examination, or if you have a raised PSA, then further examinations are advised. With an MRI scan, we can identify if there is a tumour, and if there is one, we organise a biopsy to get clarity about the aggressiveness of the prostate cancer.
The exact causes of prostate cancer are unknown. A number of factors are linked to the condition:
- Older age
- Family history (family members with prostate or breast cancer at a young age)
- Race
- Obesity
- Genetic conditions such as BRCA mutations
Prostate cancer: what are the main treatment types?
Low-risk prostate cancers contained within the prostate. This would be the majority of prostate cancers detected through an elevated PSA test result. They are generally not life-threatening. The best treatment for these types of cancers is called ‘active surveillance’. It means that we carefully monitor your cancer with regular PSA tests, clinical examinations, biopsies and MRI scans. The goal is to treat the cancer if it increases in amount or a more aggressive cancer is detected. Active surveillance avoids the risks associated with prostate cancer treatment such as urinary or sexual symptoms. If you live an active lifestyle, have small amounts of non-aggressive cancers (which are called Gleason 3+3=6 or Grade Group 1) contained within your prostate with a low PSA, then active surveillance could be the chosen path. The other treatment options such as surgery or radiation are generally not recommended due to their potential side effects and considered with more serious development of prostate cancers or increases in the amount of the cancer within the prostate gland. Intermediate or high-risk prostate cancers contained within the prostate gland. For these cancers there are two types of treatment options:- radical prostatectomy (surgically removing the prostate)
- radiation therapy
Radical prostatectomy
A surgical procedure where the entire prostate gland including the seminal vesicles is removed. If you have high-risk prostate cancer or in some intermediate-risk prostate cancers some of the lymph glands in your pelvis (which drain the prostate cancer) may also need to be removed. I perform prostate cancer surgery either robotic surgery or as traditional, open surgery. Open radical prostatectomy requires an incision in your lower abdomen, while robotic prostatectomy is performed using a minimally invasive technique through much smaller incisions. Both open and robotic radical prostatectomy have shown to have equally good cancer control and also functional outcomes including urinary control and functional outcomes. However, robotic radical prostatectomy offers a minimally invasive approach with faster recovery and better visualisation with 3D visualisation of the prostate gland and the nerves for the surgeon and is rapidly becoming standard of care throughout the world. Possible problems after surgery include urinary leakage, impotence, slight shortening of the penis and hernias.Radiation
Radiation therapy uses high energy X rays or other radiation to destroy the prostate cancer cells and is advancing rapidly with newer techniques allowing for more focused and targeted treatment of the prostate gland. This may be combined with brachytherapy (radioactive seeds) which are inserted into your prostate to give a high dose of radiation to the prostate. Generally, radiation treatments are given 5 days a week for several weeks and you may also require hormone therapy for between 6 months to 2 years especially if you have high-risk prostate cancer. There are newer fractionated therapies that combine high doses of radiation over a shorter period of time. Possible problems after radiation include urinary problems and bowel problems including needing to pass urine often, blood in stool and urine, impotence and the problems can get worse over time. There is also a small increase in bowel and bladder cancers associated with radiation.Other treatment types
Beyond the most commonly known treatment types described above, there are a few more treatments for prostate cancer. Thermal therapies HIFU (High-Intensity Focal Ultrasound) uses high intensity focused ultrasound energy waves to destroy prostate cancers by using heat. Cryoablation on the other hand uses probes to freeze the prostate cancer cells and destroy them. The techniques can also cause urinary problems and can cause serious issues if the cancer comes back. As a urologist, I generally do not recommend these therapies as first-line treatment in patients who are treated with the aim of cure. There limited data and if the cancer comes back it can be very difficult to treat with surgery or radiation. Therefore techniques are usually reserved for very select patients. Hormonal therapies Hormonal prostate cancer therapies are also called Androgen Deprivation Therapy (ADT). What they do is block or oppose the male sex hormones. These hormones drive the prostate cancer cells and the therapy stops the cells from growing. There are a number of different hormonal therapies. They can be useful in combination with radiation therapy, or in patients with cancer that has spread outside of the prostate (metastatic disease). It must be said that hormone therapies are associated with side effects:- Hot flushes
- Weight gain
- Lack of sexual drive
- Weak bones
- Memory impairment
- Cardiovascular disease
Additional support for prostate cancer
If you are diagnosed with prostate cancer, it is important to seek help from a multi-disciplinary team of specialist doctors: the GP, the urologist and the radiation oncologist work together with a prostate cancer nurse and physiotherapist to achieve the best possible results.Urologist in Melbourne for prostate conditions
Why A/Prof Weranja for prostate conditions

‘My philosophy is to treat you as a person rather than a case of the disease. So I am here to understand what is important to you. My mission is to provide you with the best available treatment so we achieve the best possible long-term outcomes.’
It’s not just about the results in themselves – it is about your quality of life.
As an accomplished academic surgeon, I use my insights into the most cutting-edge research in prostate conditions. I work with you to make sure we discuss your needs.
We then focus on providing you with the highest level, most individualised care. It is always tailored to your needs and your situation.
I build on extensive experience in both open surgery and minimally invasive surgery. That helps to aim for the best possible treatment and the fastest, more comfortable recovery.
I was trained as a urologic surgeon in Australia and spent 2 additional training years at the University of Texas MD Anderson Cancer Center. It is ranked the number 1 cancer centre in the US and it has one of the highest volumes of robotic and complex surgeries in the United States. The bottom line is that I gained extensive advanced surgical training in robotic prostate surgery. In addition, my experience also covers other minimally invasive and open urologic cancer surgery.
I truly believe that your treatment is a journey we go on together. To me, that means I provide you with the best multi-disciplinary approach to make each step as comfortable as possible. From diagnosis, treatment to post-treatment. Even if the road is difficult, I am here to offer my expertise and to support you as much as possible.

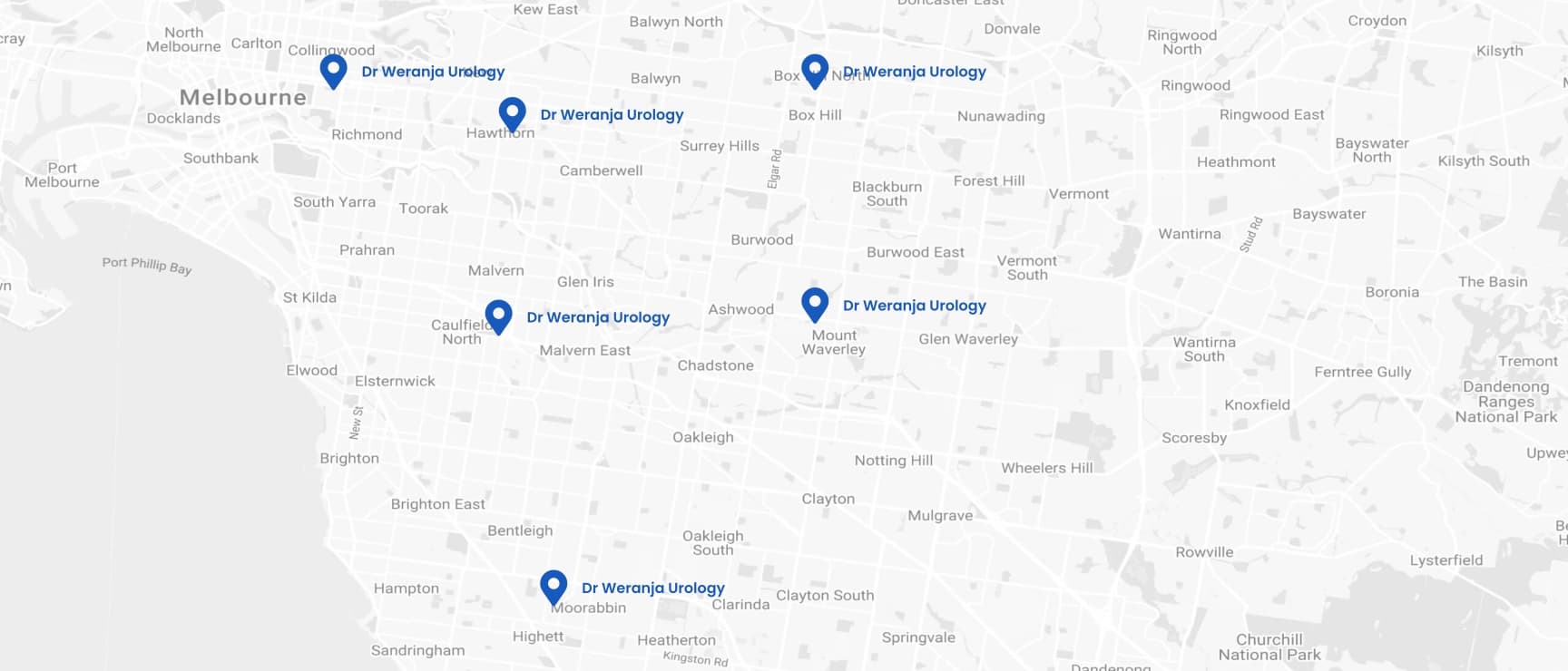
- Camberwell Road Specialists and Allied Health
- Ground floor, 124 - 126 Camberwell Road
- Hawthorn East VIC 3123
- Waverley Private Hospital
- 343-357 Blackburn Road
- MOUNT WAVERLEY VIC 3149
- Holmesglen Private Hospital
- 490 South Road, Suite A1,
Moorabbin VIC 3189
- Epworth Eastern Hospital,
- 1 Arnold St,
- Box Hill VIC 3128
- Epworth Freemasons Medical Centre
- 320 Victoria Parade,
1st Floor, Suite 103
East Melbourne VIC 3002
- Cabrini Hospital Malvern,
- 181/183 Wattletree Rd,
- Malvern VIC 3144