Urology topics for Melbourne GPs
Urology topics for Melbourne GPs
On this page
I strongly believe in the importance of our communication process and I welcome your questions. As a GP, simply email me via GPs@drweranjaurology.com.au if you have any questions about patients with urologic conditions. For urgent queries or appointments, please contact my rooms. Below I discuss some of the common topics and tips, in managing patients with urologic conditions as well as workup information for your patient referrals.
Common topics and tips in managing patients with urologic conditions
For GPs: Prostate cancer
Prostate cancer
PSA screening
- The larger, well-designed randomized controlled ERSPC trial with long-term follow-up provided Level 1 evidence that screening reduced prostate cancer mortality by 21% at 13 years of follow-up. That is for every 781 men screened, 27 men that are diagnosed with prostate cancer, and one life is saved.
- The majority of the guidelines, including the US Preventative Task Force (who previously recommended against screening) now recommend PSA screening in appropriately counselled men with a life expectancy of greater than 7 years.
- The use of newer techniques and technology such as MRI and transperineal biopsy allows for improved diagnoses of prostate cancer and select out the patients with low-risk prostate cancers who could be managed with active surveillance to potentially reduce the previously associated harms.
Who should be screened?
- Aged between 50 and 69: Offer PSA test every 2 years. If PSA levels exceed 3.0 ng/mL, offer further investigation.
- Younger than 50 and concerned about their risk for prostate cancer: Offer a PSA test every 2 years between the ages of 45 to 49. Base the testing on the initial PSA and the percentile for age *:
- ≤ 75th percentile for age: No further testing needed until 50.
- 75th and 95th percentile for age: Offer to test every 2 years.
- > 95th percentile for age: Offer further investigation.
- Then offer testing from age 50 years according to the protocol for all other men who are at average risk of prostate cancer ie every 2 years.
- Over 70 and with a life expectancy <7 years: Harms of screening may outweigh the benefits.
- 1 first degree family member (eg: a brother) diagnosed with prostate cancer at < 60 years: Offer testing every 2 years from age 45–69 years.
- Multiple first-degree family members (e.g. father and two brothers diagnosed with prostate cancer): Offer testing every 2 years from age 40–69 years. Base the testing according to the initial PSA and the percentile for age* :
- ≤ 75th percentile for age: No further testing until age 50.
- 75th – 95th percentile for age: Offer testing every 2 years.
- >95th percentile (before age 50 years): Offer further investigation.
- Then offer testing from age 50 years according to the protocol for all other men who are at average risk of prostate cancer ie every 2 years.
- In asymptomatic men undergoing screening, a digital rectal examination is not recommended as a routine addition to PSA testing in the primary care setting.
Tips to aid PSA screening
- Don’t forget to double the PSA value if on Finasteride / dutasteride / Duodart as these reduce the PSA levels by 50% (Tamsulosin does not affect PSA)
- Exclude and inform patients of the other causes of an elevated PSA
- Age-specific PSA levels may be useful but usually PSA >3 can be abnormal. Here is a general guide to some age-specific cut-offs but these can be affected by ethnicity, prostate volume and other factors:
- Ages 40-49 – 2.5
- Ages 50-59 – 3.5
- Ages 60 -69 – 4.5
- Ages >70 – 6.5
- Patients with a strong family history of breast and ovarian cancers are also at high risk for prostate cancer and may also need genetic counselling for mutations in genes such as BRCA
My suggested workup
- If an elevated PSA, repeat PSA at least 4 weeks later as a single test may be spurious.
- Free: total PSA if the PSA is between 4-10
- Perform an MSU to exclude a UTI and treat any UTI prior to repeating PSA.
- Antibiotic use for a raised PSA in asymptomatic men is unlikely to be beneficial.
- Ultrasound KUB as an initial test is not required in asymptomatic men with a raised PSA
* Resources regarding PSA counselling or a new diagnosis of prostate cancer: Understanding Prostate cancer – General Prostate Awareness Information

For GPs: Lower urinary tract symptoms
Lower urinary tract symptoms in men
My suggested workup
- Urine MCS to exclude a UTI
- Renal tract US to assess prostate volume and post-void residual
- PSA
- Creatinine/eGFR
When to refer to a urologist
It is reasonable to start patients with bothersome LUTS due to BPH on Tamsulosin as initial therapy, after discussing side effects such as postural hypotension, retrograde ejaculation. If a storage LUTS component is also present with low post void residuals, an anticholinergic therapy such as Ditropan may be considered (side effects include dry eyes, dry mouth, constipation etc,).
If the patient has ongoing symptoms or retention despite medical therapy, cannot tolerate the side effects of therapy or has recurrent UTIs, hydronephrosis or renal impairment associated with BPH, patients can be referred to a urologist for further treatment.
For GPs: Hematuria
Hematuria workup
Up to 10% of patients with hematuria (13.2% macroscopic and 3.1% with microscopic hematuria) have a urinary tract malignancy. Therefore, patients with gross hematuria and patients with asymptomatic microscopic hematuria in whom a benign cause has been excluded need further evaluation. I use a risk-stratified approach to haematuria workup as advocated by the AUA guidelines.
Useful tips in the hematuria evaluation
- Microhematuria is defined as ≥3 red blood cells per high-power field on microscopic evaluation of a single, properly collected urine specimen
- Urine dipstick is not sufficient for detection of microscopic hematuria and urinalysis and culture should be performed.
- Patients on anticoagulation therapy or antiplatelet therapy with microscopic or microscopic hematuria should have a haematuria evaluation similar to those not on these therapies
- If a benign cause of hematuria is identified for the hematuria, repeat urinalysis should be performed after treatment or resolution of hematuria
My suggested workup
- Urinalysis and urine microscopy – Also look for proteinuria or casts which could be a nephrologic cause
- Renal function tests
- Urine cytology x3
- Imaging (risk-stratified)
- Low risk – Consider USS
(Males <40yrs, Females <50s, Never smoker, microhematuria in one UA, No risk factors for urothelial cancer such as occupational exposure industrial chemical or textile dyes, Family history of urothelial cancer or Lynch syndrome, chemotherapy agents such as cyclophosphamide or isfophosphamide chemotherapy or long term catheters, stents etc.) - Others – consider CT IVP (with delayed phase) if normal renal function. If not USS will suffice.
- Low risk – Consider USS
- Referral to a urologist for cystoscopy
For GPs: Renal Colic
Renal colic
Suggested workup
- Non-contrast CT KUB. Although USS can be used to assess ureteric stones, the optimal imaging for renal colic is a CTKUB (non-pregnant patients) and provide detailed anatomy and accurately assess the stone size and site.
- X-Ray KUB. Performing an X-Ray KUB with a CTKUB for a known stone can help surveil the stone with Xray KUB rather than repeat CTs in Calcium based stones(to reduce radiation exposure) and also help determine if stones are composed of uric acid (not visualized on X-Ray KUB), where dissolution therapy can be used.
- Creatinine and renal function check
- MSU
- Emergencies associated with ureteric stones are fevers or urinary tract infections in the presence of a ureteric stone, solitary kidney with a stone, or bilateral ureteric stones. These patients need urgent evaluation and intervention and refer to the ED for urgent medical care.
Stone prevention
- One of the essential aspects of stone management is the prevention of further development of renal stones. Studies have demonstrated that 25-50% of patients will develop a recurrent stone at 5 years
- Common strategies which you could advise patients regarding stone prevention are here
- Specific tests useful tips are:
- If the patient passes a stone send for stone analysis to check composition
- Check serum Na, K, Ca, Mg, Phosphate and uric acid levels for reversible causes. (PTH if evidence of hypercalcemia)
- Check 24-hour urine collection to assess urine composition
- Refer to a renal physician if any abnormalities are found to discuss correction of metabolic abnormalities
Stent symptom management
Ureteric stents or JJ stents are placed in patients as short-term or long-term measures for various urologic conditions. Here are some frequently asked questions about them.
- Some common stent symptoms include hematuria, flank pain on passing urine, and urinary urgency.
- Some patients can have severe stent-related pain. Some medications have shown benefit in improving stent-related symptoms. These include:
- Alpha-blockers – Tamsulosin
- Anticholinergics- Vesicare
- NSAIDs
- Try to avoid opioid analgesics if possible.
- Long-term stents should also be changed every 3-6 months to prevent blockage, encrustation and stone formation.
For GPs: Renal Masses
Renal Masses
Suggested workup
- Serum creatinine and renal function test
- Triple phase CT is the gold standard for renal masses (includes non-contrast, portal venous / corticomedullary and delayed phases). Alternative options can be MRI (or USS) in patients with impaired renal function or pregnant patients.
Follow up of Renal cysts
Renal cysts are initially classified according to the Bosniak classification on a CT or MRI (to assess enhancement) rather than USS. After initial classification of renal cysts, is determined on the Bosniak score, and USS may be useful in this setting to reduce radiation exposure.
Bosniak I (simple cyst) or Bosniak II – Do not require follow-up. Malignancy risk 0%
Bosniak IIF – Large majority are benign but require imaging at 6 months and 12 months then annually for 5 years
Bosniak III and IV – Have intermediate risk or mostly malignant and need a referral to a urologist.
Useful general urologic resources for GPs Melbourne
Other useful resources
Other useful general urologic and procedural related resources for patients can be found on:
www.baus.org.uk/patients/default.aspx
www.urologyhealth.org/educational-resources?product_format=466%7c&language=1122%7c
A/Prof Weranja Ranasinghe | Urologist Melbourne
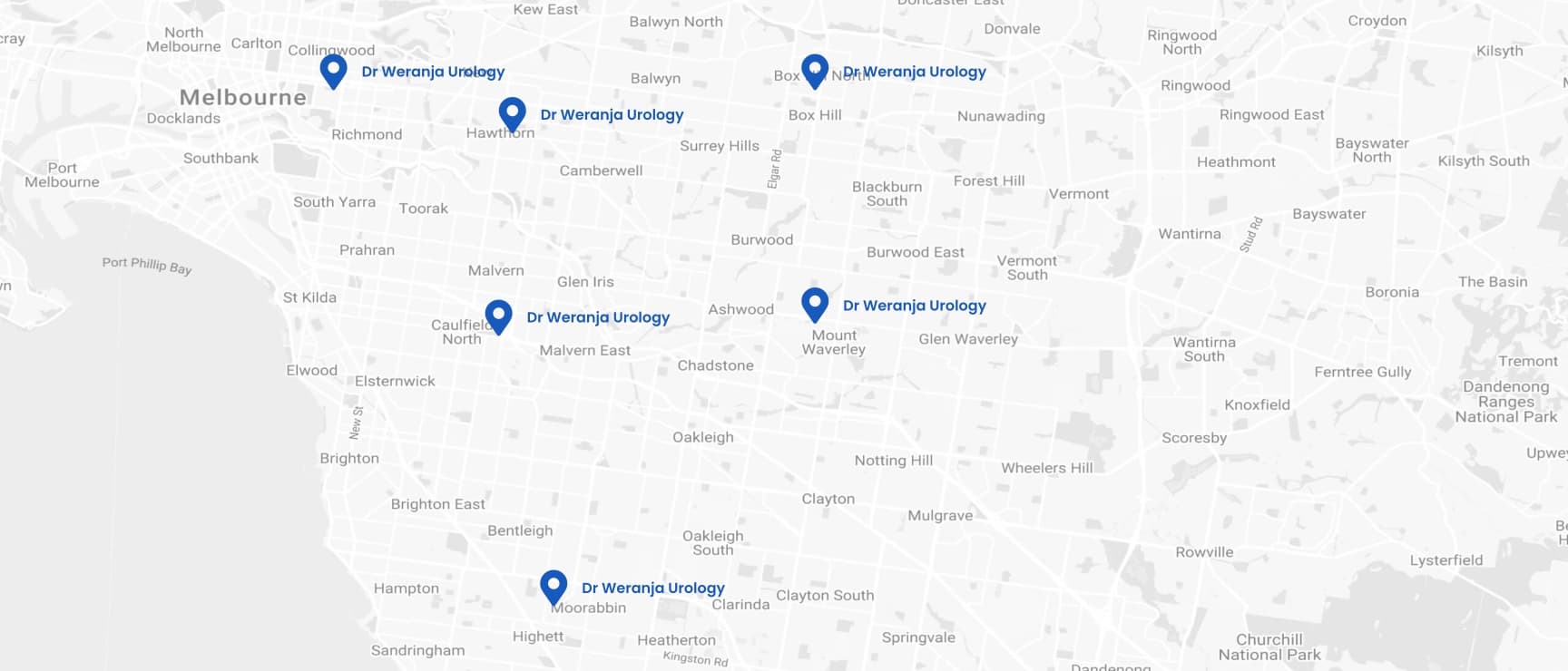
How to contact A/Prof Weranja as a GP?
As a GP you need reliable and clear communication.
If you need assistance to help your patients with urological symptoms or conditions, please contact me via this dedicated GP email inbox: GPs@drweranjaurology.com.au .
Please contact my rooms if your query is urgent. I look forward to helping you and your patients.

- Camberwell Road Specialists and Allied Health
- Ground floor, 124 - 126 Camberwell Road
- Hawthorn East VIC 3123
- Waverley Private Hospital
- 343-357 Blackburn Road
- MOUNT WAVERLEY VIC 3149
- Holmesglen Private Hospital
- 490 South Road, Suite A1,
Moorabbin VIC 3189
- Epworth Eastern Hospital,
- 1 Arnold St,
- Box Hill VIC 3128
- Epworth Freemasons Medical Centre
- 320 Victoria Parade,
1st Floor, Suite 103
East Melbourne VIC 3002
- Cabrini Hospital Malvern,
- 181/183 Wattletree Rd,
- Malvern VIC 3144